In the month of March of 2021, Lancet Psychiatry published a piece on the relationship between mental health and Covid-19 amongst the large population of low income and middle-income countries, titled ‘COVID-19 mental health impact and responses in low-income and middle-income countries: reimagining global mental health’. This article attempts to summarise the research and findings.
While mental health implications of COVID-19 in high-income countries (HICs) have been explored, there has been a dearth of attention paid to low-income and middle-income countries (LMICs). The reason this should matter is primarily that 83% of the global population live in LMICs and despite this, they have been receiving a small fraction of global health resources for mental health.
Apart from the direct health effects of COVID-19, the ramifications to contain the pandemic, with lockdowns, school closures, and curtailed livelihood opportunities have had a devastating and long-lasting effect on those in LMICs. Especially, when the most vulnerable communities in these countries have weak social safety nets and live a hand-to-mouth existence. A recent report titled ‘State of Working India – 2021, One year of Covid-19’ published by Azim Premji University shows that 230 million people have been pushed back into poverty and this is in India alone.
Short-term Impacts
This research exposes the widening of the treatment gap in mental health across LMICs, caused by the COVID-19 pandemic. The immediate impacts of the pandemic have been reported as the increase in symptoms of mental health distress, which reflect a normative response to the unexpected events and difficulties experienced by populations. In LMICs, distress due to uncertainties about the spread of the disease, the failing containment strategies, and the uncertainty of when normal everyday life will return have been at close to the population scale. Even health-care staff have fallen victim to this as reports have documented increased psychological distress, which is associated with stigma and fear of the disease, which could imply a consequent increase in the prevalence of clinically significant mental health problems. A nationwide online study of over 10000 individuals in Bangladesh reported a 33% prevalence of depression and 5% prevalence of suicidal ideation. Other vulnerable groups such as prisoners, psychiatric patients in care homes and centers, people with disabilities, and women experiencing violence or abuse, may be at greater risks of psychological distress due to pre-existing failures in human rights protection, thereby adding one more layer of complexity to mental health consequences related to COVID-19.
Long-term Impacts
This research highlights the repercussions the COVID-19 pandemic is expected to have worldwide on social determinants of health in the long term. According to the Global Burden of Disease study, mental health conditions that are most susceptible to negative social determinants are anxiety, mood, and disorders related to trauma and stress, already contributing to a disability, worldwide. This pandemic is laying the foundations for a potential worldwide suicide increase as a result of increased exposure to known risk factors, such as economic stress job insecurity and unemployment, social isolation, decreased access to community support, barriers to mental health treatment, and exacerbated physical health problems. While a model combining data from multiple countries, including both HICs and LMICs, suggests that job losses due to the pandemic might result in up to 9570 additional suicides per year, globally, no such models exist for LMICs alone. This is troubling, especially since LMICs bear the bulk of the global burden of suicide and are more vulnerable to economic devastation from the pandemic. Which has in fact been supported by a review on Indian media on this pandemic and suicide.
Children’s Mental Health
The article talks about the profound effect school closures for such a long period of time will have on the mental health of children, adolescents, and young adults globally. Schools play an integral part in shaping the mental wellbeing of young people by providing a space for socioemotional development, friendship and social support networks, protection from risk-taking behaviors’ and exploitative labor, delays to early marriage and childbearing. It also acts as a guard to detect and intervene early to prevent and reduce child abuse at home. In a lot of LMICs, schools are a key access point for food for children, which further promotes academic performance and cognitive development. School closures due to this pandemic have not only stripped children of their access to education but have the unintended consequence of food insecurity, which negatively affects mental health.
Response to Mental Health Needs
Due to the progressing nature of the pandemic in many countries, there is little evidence of the impact of mental health programs. Moreover, their implementation under real-world emergency circumstances with no resources for evaluation, there has been insufficient time to complete comprehensive evaluations.
- Governments in LMICs have taken the initiative to develop COVID-19 mental health plans, along with launching and implementing diverse programs addressing population-level and individual clinical needs
- The authors stress the need to focus on evaluating these programs for the future such as low-cost positive psychology approaches addressing population mental health needs
- Growing efforts to develop international guidance, national policies, and resources for LMICs to address mental health and psychosocial support (MPHSS) needs as shown in figure 1
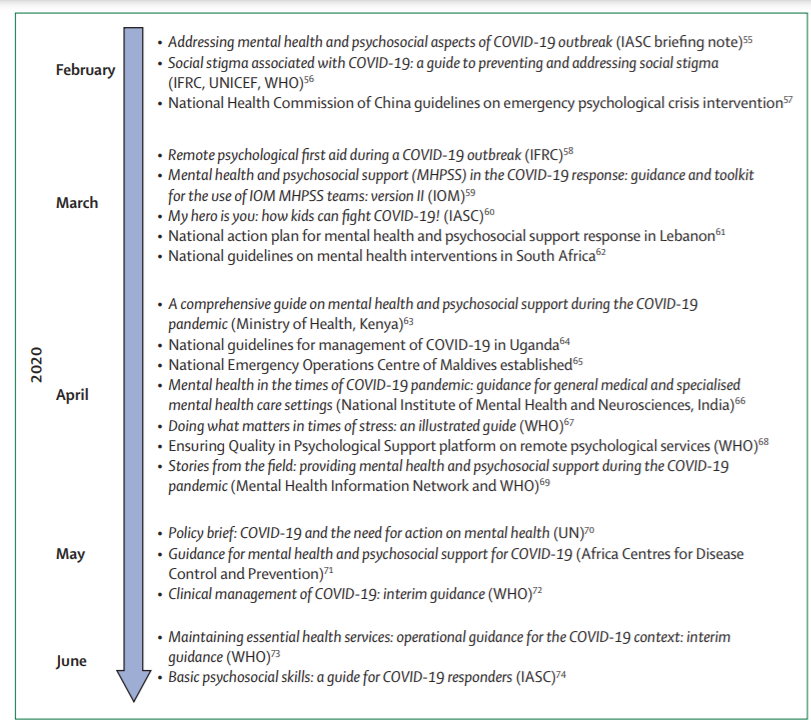
Figure 1: Timeline of mental health and psychosocial support guidance, policies, and resources in LMICs during the initial months of the Covid-19 pandemic
IASC – Inter-Agency Standing Committee
IFRC – International Federation of Red Cross and Red Crescent Societies
IOM – International Organization for Migration
- Members of the healthcare system, ranging from community health workers to mental health specialists, have been trained to help detect individuals with mental illness and psychological distress
- Innovating responses were documented across many LMICs, such as fairy tales being read to children, phone helplines, home outreach programs, training, and capacity building programs in areas on providing mental health support, child-friendly protocols, and the like, depicted in figure 2
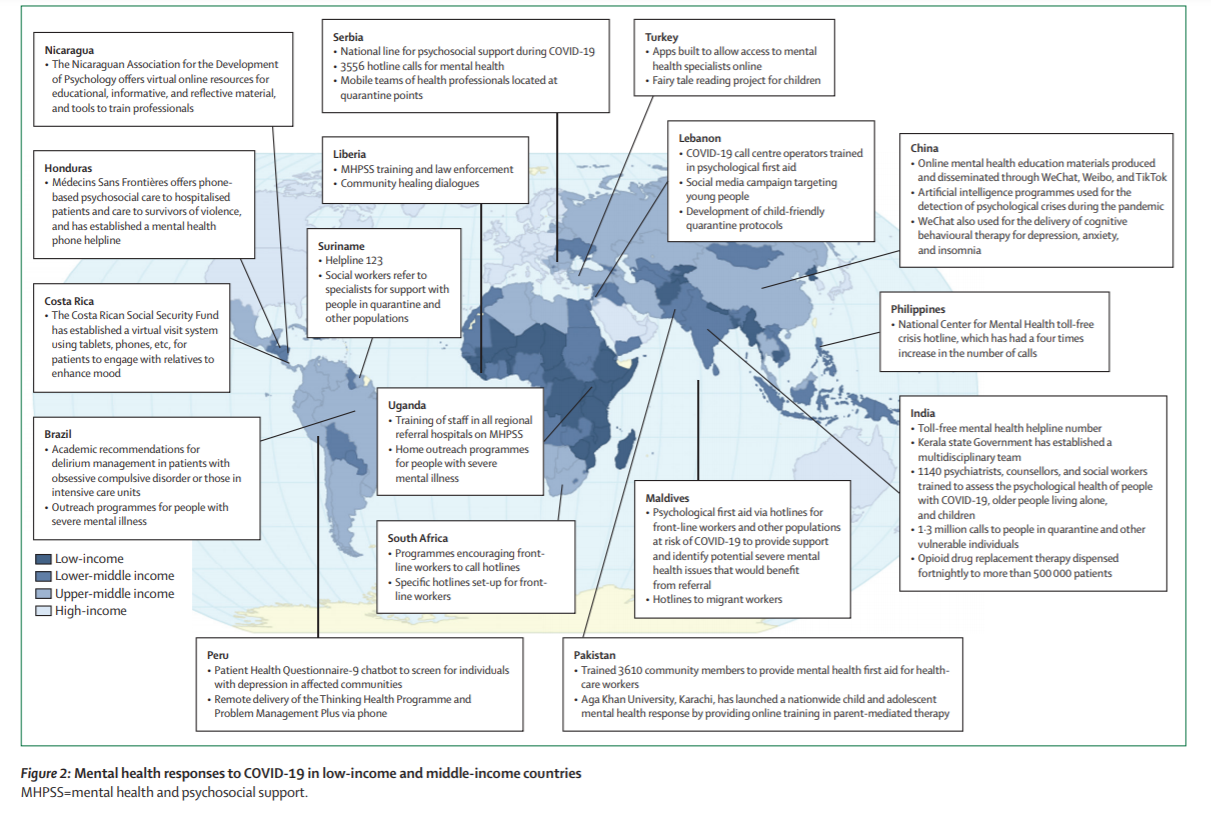
Figure 2: Mental health responses to Covid-19 in low-income and middle-income countries
MHPSS=Mental Health and Psychosocial Support
- A major initiative has been building capacities among non-specialists in the field to deliver psychological services remotely. Problem Management Plus, a five-session psychological intervention based on problem-solving therapy, designed for delivery by non-specialists in humanitarian settings has been adapted for remote training and delivery through voice-only phones or videos by the International Federation of Red Cross and Red Crescent Societies (IFRC) in East African countries
- Based on the large and growing demand for psychological services to be delivered remotely, the World Health Organisation (WHO) has adapted the Ensuring Quality in Psychological Support (EQUIP) platform, which includes guidance on preparing for remote delivery and managing suicidality in remote delivery, as well as a competency assessment tool to support the safe delivery of psychological services
- Face-face services have been maintained in parts of some LMICs, indicating considerable variability in the response of the mental health-care system (for example, in Punjab, India, opioid drug replacement therapy was successfully implemented, in Brazil, a hybrid model of in-person and remote services was instituted for individuals with psychotic disorders, including injections delivered during in-home visits, where food security was also monitored), as shown in figure 3
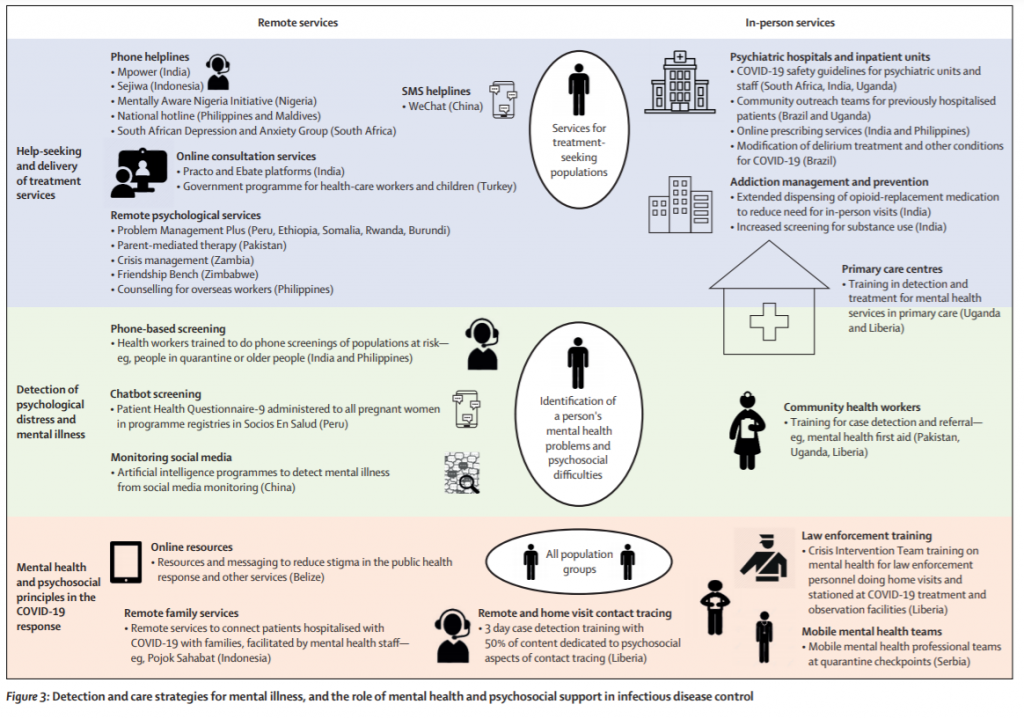
Figure 3: Detection and care strategies for mental illness, and the role of mental health and psychosocial support in infectious disease control
Inequitable Distribution of Responses
Unfortunately, the access to all these interventions and responses is not equitably distributed due to settings with restricted phones, electricity, or Wi-Fi access. People with disabilities often encounter practical barriers to accessing support and many of these interventions are not accessible to those with sensory impairments. Children and adolescents miss out on mental health care which would have otherwise been delivered via school counsellors or student health services.
Recommendations to build better Global Mental Health Services.
- Integrating mental health services into Universal Health Coverage (UHC)
- Improving access and coverage of psychosocial interventions
- Elimination coercion in mental health care
- Integrating mental health interventions into other sectors
- Addressing the mental health of children and young people
- Incorporating technological innovations in mental health services
This piece of research throws light on the urgent necessity for countries to respond to this global phenomenon which is unlike any other in human history, where the evidence points to large and long-lasting mental health impacts, in under-resourced contexts and disadvantaged populations. While exploring various interventions and understanding their limitations, the emphasis is laid on countries to reassess how human society organises itself to recover from these impacts, by investing in building mental health systems. The aim is not only to reimagine mental health care in LMICs but also to reframe mental health as an area of priority in countries all over the world.
Anjali Paul,
Content Writer




